By Vernell Burris, Jr.
(Stage 4 Oligometastatic Prostate Cancer Patient)
For too long, prostate health has been a conversation we’d rather not have. But as Black men, we don’t have the luxury of ignoring it. The numbers don’t lie—prostate cancer disproportionately affects us, and if we’re not proactive, we put our lives on the line. Dr. Thomas Emerson, a leading urologist with Wellstar Health System and a Fellow of the American College of Surgeons, breaks it down for us—what we need to know, when to get screened, and how to stay ahead of the game.
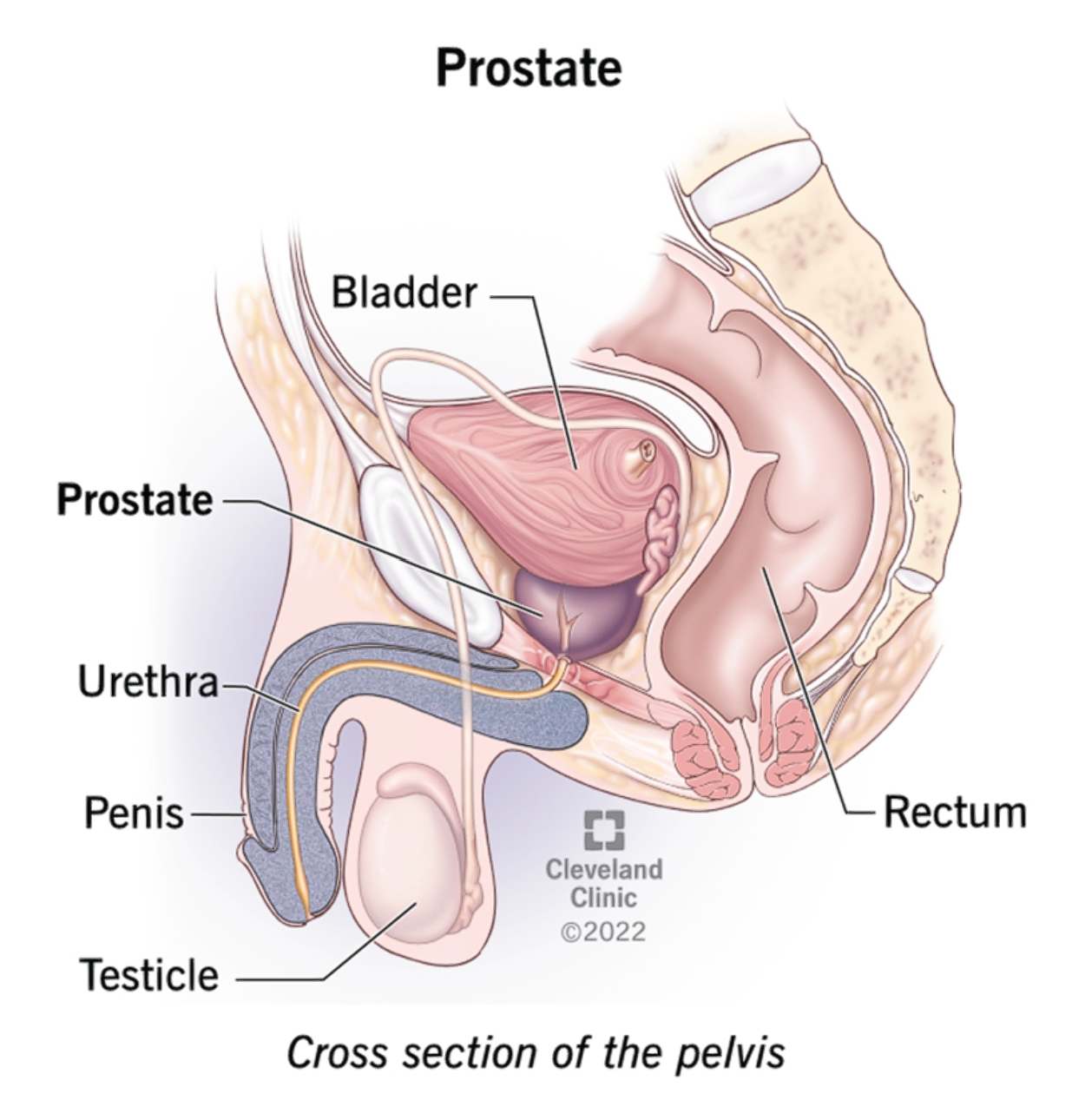
What Does the Prostate Actually Do?
Fellas, let’s start with the basics. The prostate sits at the base of your bladder and surrounds the urethra—the tube you urinate through. When you’re young, it plays a big role in fertility, producing enzymes that help sperm survive and do their job. But as you age, the prostate becomes more of a liability than an asset. It can become inflamed, enlarged (making it harder to urinate), or develop cancer.
If the prostate were as easy to remove as an appendix or tonsils, doctors might do it at the first sign of trouble. But because of its location, that’s not an option unless absolutely necessary. That’s why knowing the risks and getting ahead of potential problems is critical.
When Should You Get Screened?
General medical guidelines recommend prostate cancer screening between ages 50 and 55. But if you’re a Black man, listen up—your clock starts ticking earlier. Because high-grade prostate cancer hits us sooner and more aggressively, screenings should begin at age 40. If you have a family history of prostate cancer, it’s even more urgent.
Understanding PSA Testing
Prostate-Specific Antigen (PSA) testing isn’t a direct cancer test, but it’s a crucial tool in detecting potential problems. A PSA level under 4 ng/mL is generally considered normal, but this varies with age. Early detection of high-grade cancers significantly improves survival rates, so don’t skip out on this important test.
The Role of Genetics and Family History
Only about 10% of prostate cancer cases are genetic, but if your family history includes prostate, colon, breast, ovarian, or pancreatic cancer, you need to take extra precautions. Genetic testing can provide valuable insights, and if you have a predisposition, encourage your brothers, sons, and nephews to get checked, too.
Why Black Men Are at Higher Risk
Age, ancestry, and ethnicity all play a role in prostate cancer risk. African American men are more likely to develop high-grade prostate cancer at a younger age, and if left undetected, it becomes harder to treat. But here’s the good news—early detection has led to a dramatic drop in prostate cancer deaths, especially among Black men who take action early.

Your Diet Matters More Than You Think
One of the most overlooked aspects of prostate health is what’s on your plate. Studies show that men in Japan—who consume diets rich in fish, soy, and antioxidants—have much lower rates of prostate cancer. The takeaway? Cut back on red meat, dairy, and unhealthy fats. Instead, load up on foods high in antioxidants—tomatoes (lycopene), soy (isoflavones), and ground flaxseed. Even for men already diagnosed with prostate cancer, the right diet can help slow its progression.
Taking Decisive Action Can Save Your Life
If you’re diagnosed with prostate cancer, early treatment can make all the difference. While there’s always a risk that cancer cells could spread undetected, catching it early gives you the best shot at survival.
Be Proactive, Stay Alive
The statistics don’t lie—prostate cancer deaths have dropped significantly over the last 30 years, and early screening has made a massive impact. Black men who prioritize their health stand a much better chance of beating this disease. Don’t wait until it’s too late. Talk to your doctor, get screened, and encourage the men around you to do the same.
About Thomas Emerson, MD
Dr. Emerson graduated from Georgia State University in Atlanta and received his medical degree from the Medical College of Georgia in Augusta. He completed his general surgery residency at the Medical Center of Central Georgia and his urology residency at Ochsner Clinic in New Orleans.








